Understanding Autism Insurance Coverage in Texas
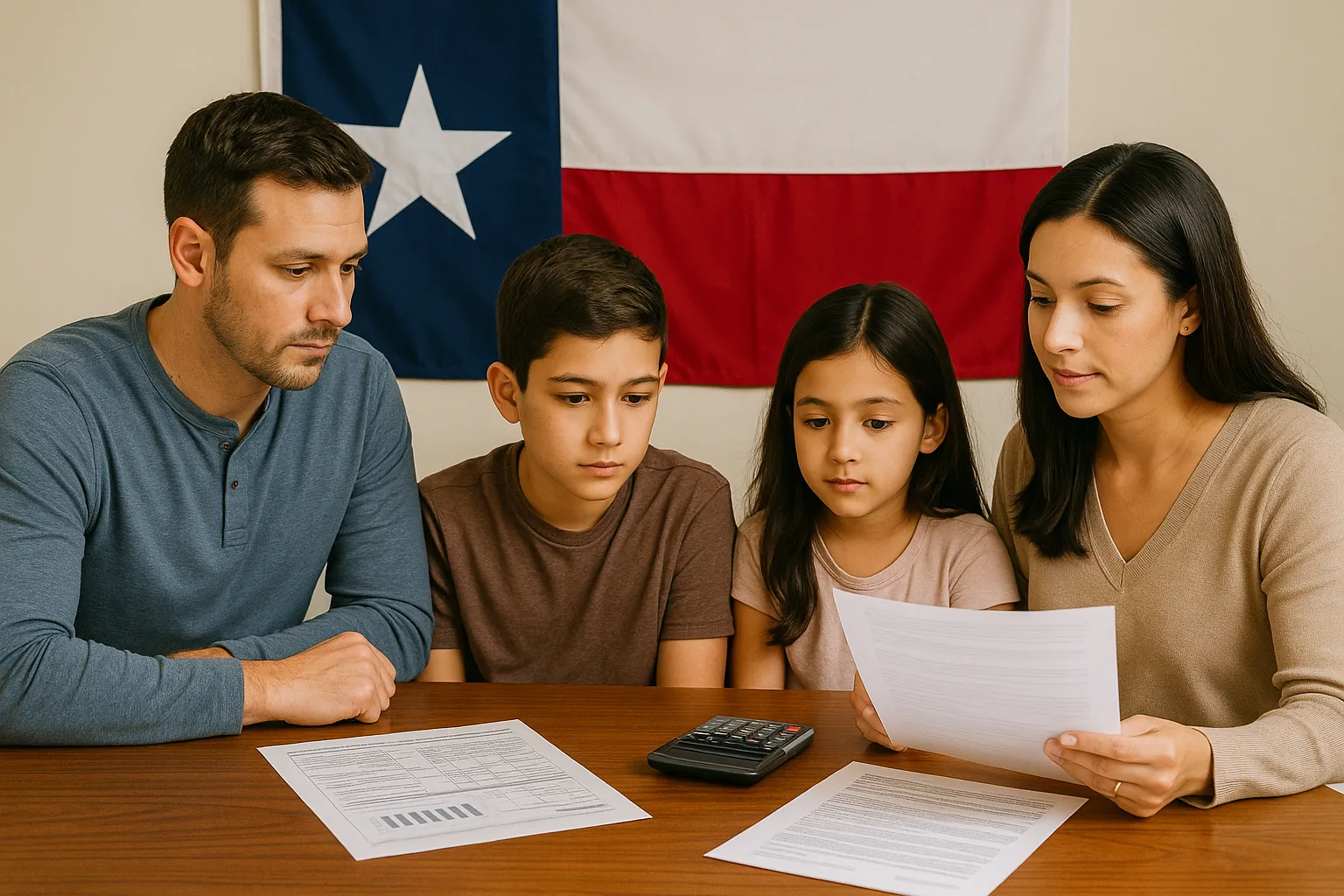
For many families, working to get autism insurance coverage in Texas is one of the biggest hurdles when first starting ABA therapy. Sorting through all the different types of plans, buzzwords, and rules can feel overwhelming.
Fortunately, insurance coverage in Texas has improved tremendously, making it easier than ever to get ABA therapy covered. But, keep in mind that rules can still vary depending on what insurance plan you have.
This article will help clarify the most confusing parts of getting ABA therapy covered by insurance such as:
- which insurance plans must cover ABA therapy
- how Texas laws affect insurance coverage
- what limitations families may encounter
- what steps you can take to avoid unexpected costs
Key Takeaways: Autism Insurance Coverage in Texas
- In Texas, many insurance plans are required to cover autism evaluations and medically-necessary ABA therapy.
- Coverage may vary depending on what kind of plan you have.
- Medicaid in Texas covers ABA therapy, however the availability will depend on several things like approval timelines and provider capacity.
- No matter what insurance plan you have, you can expect to encounter some obstacles like prior authorizations or periodic therapy plan reviews. These can often be reversed through appeals, provider support, and updated clinical documentation.
What Autism Insurance Coverage Includes in Texas
In Texas, fully-funded insurance plans must cover generally recognized services for autism such as:
- evaluation and assessment
- applied behavior analysis
- speech and occupational therapy
- physical therapy
- behavior training/management
- medications and/or supplements intended as a therapy for autism
In short, these types of plans usually cover evaluations and medically-necessary ABA therapy when there’s documentation of an autism diagnosis.
What are Fully-funded, Self-Funded, and Individually-Purchased Plans?
So what’s the difference between fully-funded, self-funded, and individually purchased plans? Here’s a basic overview:
- Fully-funded plan:
- In a fully-funded plan, the employer pays a premium (which is a recurring fee), while the insurance company takes care of paying claims. These plans are usually not as flexible as self-funded plans.
- In a fully-funded plan, the employer pays a premium (which is a recurring fee), while the insurance company takes care of paying claims. These plans are usually not as flexible as self-funded plans.
- Self-funded plan:
- With self-funded insurance plans, the employer sets aside a certain amount of money and pays for insurance claims. These plans are usually more flexible than fully-funded plans. In some cases, you can even get money back at the end of the year!
- With self-funded insurance plans, the employer sets aside a certain amount of money and pays for insurance claims. These plans are usually more flexible than fully-funded plans. In some cases, you can even get money back at the end of the year!
- Individually-purchased plan:
- Individual health insurance plans are not offered through an employer, which means you need to purchase them yourself. Although this offers a lot of flexibility, it also means that the terms and conditions of each plan can vary quite a lot.
When it comes to getting covered for ABA, the type of plan matters because fully-funded plans are generally required to cover autism therapies in Texas.
Understanding the Texas Autism Insurance Mandate
The Texas Autism Insurance Equity Act is a law that helps families get insurance coverage for autism therapies.
This law requires many insurance plans to, at minimum, cover autism therapies, such as ABA therapy. There are two important rules/restrictions:
- the diagnosis of autism must be in place before the child’s 10th birthday
- there is a $36,000 per year maximum coverage limit
This matters because more families today are able to get coverage for the care they need. It allows more plans to cover medically-necessary therapies like ABA. Medically-necessary is defined in Texas as “treatments for conditions that cause suffering or pain, cause physical deformity or limitations in function.”
It also removes some of the older age-based restrictions that made care harder to access.
Although this mandate makes it easier to get insurance coverage, it does not guarantee that every plan will have the same benefits. Some plans may still have coverage limits or reassessment requirements.
Private Insurance vs Medicaid in Texas
Other important types of health insurance in Texas to understand are private insurance and Medicaid.
Private insurance plans are offered by employers. Usually these plans have higher premiums and overall costs. One perk is that the care provider network is usually larger, meaning you have more options. However, one drawback is that these plans vary a lot more in what benefits they provide.
Medicaid is a low-cost insurance program offered to people who meet low-income eligibility requirements. The biggest benefit of Medicaid plans is that they are lower cost, with less out-of-pocket fees. However, there may be more limited in-network provider options.
Medicaid insurance in Texas now covers ABA. However, some important things to consider with this program are provider availability, location, and approval timelines.
No matter what insurance plan you have, try to keep realistic expectations. It’s not uncommon for the process to include bumps in the road like waitlists, paperwork, and periodic authorization reviews.
What to Expect Before Starting Insurance-Covered ABA in Texas
Many plans have certain requirements before starting insurance coverage for ABA. Here’s what to expect:
- formal documentation of an autism diagnosis
- documentation of medical necessity
In addition, many insurers require prior authorization, which just means getting your coverage approved before you actually start ABA. They may also ask for updated therapy plans at regular intervals in order to keep covering the therapy.
While these may all seem like even more barriers for your family, they’re just standard practices meant to verify therapy eligibility and make sure that everyone gets the appropriate care.
Not sure if all your documentation is in order? Reach out to Alpaca Health to verify your insurance benefits and get personalized support in navigating the approval process.
Common Autism Coverage Challenges (and How to Handle Them)
Sometimes the process of getting insurance coverage can be challenging. Here are some of the most common challenges and how to handle them:
Reduced Authorized Hours
Having authorized hours reduced can be very frustrating. One way to avoid this is to make sure that all of the needed documentation is up-to-date. For example, many plans require regular therapy updates. In addition, insurance plans have appeals processes where you can challenge their decisions and have them re-evaluate your situation.
Denials Due to Missing Documentation
Your care provider can help guide you and make sure that you have all the documentation you need to get approved. For example, many insurance plans require formal documentation of an autism diagnosis. Be sure to closely review all your plan’s criteria for getting covered.
Difficulty Finding In-Network Providers
Some insurance plans have very limited options for in-network providers. If you’re still deciding between insurance plans, make sure that there are a variety of in-network providers to choose from. If you qualify for Medicaid, Alpaca Health can help connect you with a wide network of ABA providers in Texas.
Because insurance is so complex, dealing with these hurdles is actually pretty common. Appeals, peer-to-peer reviews and written explanations are all just part of the process and it’s something many people go through.
If you’re still having trouble, then getting in touch with a health insurance advocate can really help. These people are knowledgeable about everything relating to insurance and are passionate about getting people the healthcare they need.
You can also look to Texas autism resources to learn about financial aid opportunities, find other programs that can help support your child, and get advice from other families who have had similar experiences.
Steps to Verify Your Autism Insurance Benefits
With all this being said, you may now be wondering what your autism insurance benefits are. Here are some steps you can take to find out what autism insurance benefits you have.
Confirm Whether ABA Is Covered
The first step is to call your insurance provider to find out if there is insurance coverage for ABA therapy. You should also ask if there are any exclusions that apply. The answer might vary depending on if your plan is fully funded or self-funded.
Ask About Authorization Requirements
It’s also important to ask if there are any authorization requirements before service starts. Oftentimes, insurance carriers need diagnostic reports and a therapy plan in order to get coverage authorized for you.
Check Provider Network Status
It’s also recommended to check whether ABA providers are considered in-network (meaning they have a contractual agreement with your insurance plan). This can help you avoid much higher fees. Out-of-network coverage is sometimes available, though there are often stricter limits.
Review Deductibles and Out-of-Pocket Limits
It’s important to be aware of your plan’s deductibles, coinsurance, and maximums. This can help your family plan for those pesky early-year expenses. Costs often decrease once the out-of-pocket limits are reached.
Autism Insurance Coverage in Texas FAQs
Do all insurance plans in Texas have to cover ABA therapy?
- According to the Texas Autism Insurance Equity Act, fully-funded health insurance plans are generally required to cover ABA under certain criteria. Other types of insurance plans may not cover ABA.
Are there age limits or annual caps for ABA coverage in Texas?
- For fully-funded plans, the maximum annual coverage limit for ABA in Texas is $36,000. There is no age-limit, however in order to be eligible for coverage, your child needs to have a formal diagnosis of autism before their 10th birthday.
What can families do if their insurance denies ABA coverage or reduces authorized hours?
- This happens a lot more than you think, so try not to get too discouraged! Fortunately, there are usually appeals processes in place to help you get the coverage you need.
How can I find out what my autism insurance benefits are?
- Get in touch with your insurance provider to find out if ABA is covered and if there are any authorization requirements.
How Alpaca Supports Families Navigating ABA Insurance Coverage in Texas
Families shouldn’t have to navigate the complicated insurance system alone. Alpaca Health streamlines the process of insurance verification in Texas, so that you can focus on your child. Whether it's checking your benefits, or connecting you with local providers, we can help you avoid surprise fees and help you get started with ABA therapy within days, not months.
All of our ABA providers make clinical decisions based on what’s best for your child, not corporate quotas. You can get flexible care to fit any schedule, whether it’s at home, school, or in-office
Connect with Alpaca Health today if you need any help understanding your insurance benefits or starting ABA therapy in Texas.
Sources:
https://www.aetna.com/employers-organizations/self-insurance-plans.html
https://www.cms.gov/medical-bill-rights/help/guides/patient-advocate
https://www.census.gov/topics/health/health-insurance/about/glossary.html
https://statutes.capitol.texas.gov/Docs/IN/htm/IN.1355.htm
https://www.autismspeaks.org/texas-state-regulated-insurance-coverage
https://www.healthinsurance.org/glossary/private-health-insurance/
https://www.texasautismsociety.org/advocacy-alert-hb-4506-autism-insurance-equity-bill/
High Quality, Local ABA
If you are ready to partner with a local BCBA and receive the highest quality of care, reach out today!